|
This material is the interaction I had about a request for an interview. Not only will, I think, the reporter help tell SETMA's story, she will also be prepared to write about us in the future, if the opportunity presents itself.
Clinical Decision Support - Request for an interview - Writer’s Goal and Questions
Dr. Holly’s Concepts about CDS and Responses to questions
June 27, 2012
Reporter’s Charge:
My assignment: This feature should illustrate the potential of clinical decision support (CDS) to standardize and improve clinical decision making at the point of care€”and profile three to five providers that are fairly advanced in using these tools to improve outcomes and reduce costs. The primary focus of this article should be on identifying current challenges to successfully implementing CDS€”and offering lessons learned for using CDS to prepare for the future of healthcare delivery.
The RWJF summary describes your use of clinical decision support so I have no additional questions about how you use it.
Reporters Original Contact
As I mentioned, I would like to interview Dr. Holly for an article in the upcoming issue of Leadership magazine, published by the Healthcare Financial Management Association, the professional association for healthcare CFOs. A link to a pdf of the most recent issue of Leadership is at http://www.hfma.org/leadership/
The article is about the use of clinical decision support systems to improve healthcare delivery in various settings. I will be including information about CDS use in a multi-hospital system, a small community hospital and a large cardiovascular practice, and I would love to include information about SETMA's use of clinical decision support as well.
Thank you for forwarding my request to Dr. Holly, and I look forward to hearing from him.
Dr. Holly Referred Reporter to website materials:
Report to Robert Wood Johnson Foundation request for material on SETMA about Primary Care Project Robert Wood Johnson Foundation Primary Care Team Learning from Effective Ambulatory Practices Measures Worksheet
Reporter’s Questions:
My questions are:
- How have you developed the CDS tools? Are some/all of these readily available in your NextGen EHR system? (I doubt it...but want to make sure) Do you have a large IT department? Please describe.
- How do you decide what tools to develop? For example, how did you decide it is worth the time/money/effort to develop a lipid disease management tool?
- Are the clinical decision support tools used on desktop computers in each exam room? Tablets that each nurse/physician carry throughout the day? Or?
- How much has SETMA invested in CDS tools?
- How have SETMA's CDS tools affected the overall cost of care? (For example, improved blood sugar levels for diabetic patients obviously reduces the cost of their care over their lifetimes. Have you considered the big-picture savings that could be attributed to your CDS tools?)
- How does the use of the pre-visit preventive and screening tool and the LESS Initiative tool affect work flow? Did you add staff to administer these tools before the patient visits the physician? How long does it take to administer each tool?
- How does the use of the disease management tools affect work flow? Do they affect the average length of an office visit?
- How have SETMA physicians reacted to the emergence of CDS tools? Universal enthusiasm? Reluctance to comply? Reticence about public reporting? Have you had any turnover among your physician or nursing colleagues that is attributable to your use of CDS tools?
- What have been the biggest challenges to using CDS tools? How have you addressed those challenges?
- What have been the biggest rewards/benefits of using CDS tools?
- What "lessons learned" can you share with other healthcare leaders that want to increase the use of CDS in the outpatient setting?
Dr. Holly’s Response to the Reporter’s e-mail about interview
I have your questions and will address them today and tomorrow. From 9-12 today, SETMA’s clinics are closed and we have a provider training course. We do this once each month. Today, we start a four-month review of the Institute for Healthcare Improvement’s (IHI) four-part series on Avoidable Rehospitalizations. This material focuses upon care coordination.
- June-- SETMA will review (slide deck) -- How to Guide: Improving Transitions from the Hospital to The Clinical Office Practice to Reduce Avoidable Rehospitalizations
- July-- SETMA will review (slide deck in preparation) -- How-to Guide: Improving Transitions from the Hospital to Post-Acute Care Settings to Reduce Avoidable Rehospitalizations
- August -- SETMA will review -- How-to Guide: Improving Transitions from the Hospital to Skilled Nursing Facilities to Reduce Avoidable Rehospitalizations
- September -- SETMA will Review -- How-to Guide: Improving Transitions from the Hospital to Home Health Care to Reduce Avoidable Rehospitalizations
Those attending will be:
- Hospital Service Team
- Healthcare Providers who follow patients in the hospital
- Care Coordination Department Members
- Administrative staff members including executive nursing staff and IT staff
- External healthcare leaders who work closely with SETMA
The following is a link to the presentation material mentioned above:
Review of Institute For Health Improvement Reducing of Avoidable Rehospitalizations Materials
Dr. Holly’s Concepts about CDS
In order for Clinical Decision Support (CDS) to contribute to the Triple Aim (Improve Care, Improve Health, Decrease Cost), CDS must be incorporated into the providers’ work flow. The success of that will be the dependent upon:
- Design - it must make the providers’ work easier rather than add to the burden of that work. We call this, “We want to make it easier to do it right than not to do it at all.” This also includes bringing to bear upon a patient encounter what is known rather what an individual provider knows.
- Deployment - the display of the CDS tools is critical. This is the distinction between electronic patient records and electronic patient management. The former is a means to the end of documenting a patient encounter; the latter is a methodology for leveraging the power of electronics to fulfill the Triple Aim. Our monthly provider training sessions is a set in the process of incorporating CDS into workflow.
- Demonstration - The ability for a provider to measure his/her performance at the point of care and of the organization to track, audit, analyze and report by provider name performance as both process and outcome. The principle is, if you make a change in work flow will it make a difference. That cannot be assumed, it must be proved. This is the fundamental change in CME methodology developed by Performance Improvement CME (PI-CME).
To this end, for our internal use, SETMA has modified the Triple Aim as follows:
- “Improve care” changed to “improved processes” - this is the CDS element of the Triple Aim and addresses the deployment of the CDS
- “Improve health” changed to “improved outcomes” - this is the Demonstration of the value of the CDS as it allows providers to improve the results of there are and to do it in a provable manner.
- “Decreased cost” changed to “sustainability” - this is the design element of CDS as it addresses whether, once the focus is not acutely on the CDS, that it will continue to be used and that it will continue to improve process and outcome. Being based on scientific evidence and best practices, CDS will be expected to decrease cost as it improves the process (care), the outcome (health) and as it contributes to sustainability (decreases cost).
Dr. Holly’s Answers to Reporters Questions
Question One -- How have you developed the CDS tools? Are some/all of these readily available in your NextGen EHR system? (I doubt it...but want to make sure) Do you have a large IT department? Please describe.
Question 1 Part I -- How? -
In 1998, we purchased the NextGen EMR. It took us until January, 1999 to develop a data base where we could document a patient encounter with the EMR We started using the EMR on Tuesday January 26, 1999. By Friday, January 29th, we were seeing ALL patients with the EMR. In May, 1999, four seminal events transformed SETMA’s healthcare vision and delivery.
First, we concluded that EHR was too hard and too expensive if all we gained was the ability to document an encounter electronically. EHR was only “worth it,” if we leveraged electronics to improve care for each patient; to eliminate errors which were dangerous to the health of our patients; and, if we could develop electronic functionalities for improving the health and the care of our patients. We also recognized that healthcare costs were out of control and that EHR could help decrease that cost while improving care. Therefore, we began designing disease-management and population-health tools, which included “follow-up documents,” allowing SETMA providers to summarize patients’ healthcare goals with personalized steps of action through which to meet those goals. We transformed our vision from how many x-rays and lab tests were done and how many patients were seen, to measurable standards of excellence of care and to actions for the reducing of the cost of care. We learned that excellence and expensive are not synonyms. We were well on our well to working toward Electronic Patient Management rather than Electronic Patient Records.
Second, from Peter Senge’s The Fifth Discipline, we defined the principles which guided our development of an EHR and the steps of our practice transformation; they were to:
- Pursue Electronic Patient Management rather than Electronic Patient Records
- Bring to every patient encounter what is known, not what a particular provider knows
- Make it easier to do “it” right than not to do it at all
- Continually challenge providers to improve their performance
- Infuse new knowledge and decision-making tools throughout an organization instantly
- Promote continuity of care with patient education, information and plans of care
- Enlist patients as partners and collaborators in their own health improvement
- Evaluate the care of patients and populations of patients longitudinally
- Audit provider performance based on endorsed quality measurement sets
- Integrate electronic tools in an intuitive fashion giving patients the benefit of expert knowledge about specific conditions
The third even was that my co-founding partner came in one day and was obviously depressed. I asked him what was wrong. He said, “We’re not evening crawling yet,” speaking of our use of the EMR. I agreed and said, “Tell me something, when you oldest child first turn over him bed did you complain that this child could not crawl but all he could do was turn over in bed?” He smiled and I continued, “You celebrated his progress didn’t you?” I concluded, “You’re right, we have a long way to go, but we have started. If in a year, we are doing no more than we are currently doing, I will join your lamentation, but today, I am celebrating that we have started.” At that moment we adopted a celebratory approach to our efforts. We compared ourselves to ourselves, just like Mikhail Baryshnikov, who said, “I never try to dance better than anyone else, I try to dance better than myself.”
The fourth seminal event was the preparation of a philosophical base for our future; developed in May, 1999, this blueprint was published in October, 1999. It was entitled, More Than a Transcription Service: Revolutionizing the Practice of Medicine With Electronic Health Records which Evolves into Electronic Patient Management”. The following excerpts are from that paper:
“...when the (EHR) encounter is completed and a copy of the record is given to the patient:
- “The patient is able to review the record, further gaining confidence that if my doctor knows all of this about me, (I can trust that my care is appropriate).
- “If any data is inaccurate or has become invalid, the patient can correct the record, becoming a partner with the provider in the process of producing a complete, accurate, valid and current medical record.
“...collaboration between every person - including the patient -- participating in the patient’s care... and the sharing of information...at every point of the patient's (care)...means that the emergency department, hospital, home health agency, hospice, physical therapy, reference laboratory and long-term care facility have...a seamless interface with the patient’s EHR.
“...in the continuum of care model...care management drives care...which is a database function. If the patient's record is available at every point of contact...there will not be:
- “Redundancy...
- “Inefficiency...
- “Excessive cost ...
“...Healthcare providers must never lose sight of the fact that they are providing care for... unique individuals... (who) deserve our respect and our best... empowering the patient to achieve the health he/she determined to have. “
These have been and are the priorities of SETMA, all require CDS. Prior to their enunciation and now pursuant to the National Strategy’s goals, SETMA has achieved:
- NCQA Tier III Patient-Centered Medical Home
- Accreditation Association of Ambulatory Healthcare accreditation for Ambulatory Care
- AAAHC accreditation as a Medical Home
- Diabetes Center of Excellence Affiliate at Southeast Texas Medical Associates
- American Diabetes Association recognized Diabetes Self-Management Education Program
- Elimination of Ethnic Disparities for diabetes and hypertension care
- Effective Transitions of Care from inpatient to ambulatory care for 25,432 inpatient admissions since July, 2009, including Medication Reconciliation; a 99.1% efficiency of delivering to the patient and/or family, a written, personalized Hospital Care Summary and Post Hospital Plan of Care and Treatment Plan at the time of discharge; first-day Post Hospital Discharge Telephone contact for a 12-30 minute Care Coaching call.
- A 22% decrease in preventable readmissions
- Improvement between 2000 to 2011 of mean HbA1cs from 7.54% to 6.65% and of standard deviations from 1.98 to 1.30.
- NCQA Diabetes Recognition Program for each of SETMA’s clinics
- Office of National Coordinator recognition as one of thirty exemplary practices in the United States for Clinical Decision Support.
- HIMSS peer-reviewed Stories of Success
- HIMSS Davies Award
- Agency for Healthcare Research and Quality publication of SETMA’s LESS Initiative (Lose Weight, Exercise & Stop Smoking) on AHRQ’s Innovations Exchange.
Question 1 Part II - NextGen
None of the tools which we have built are a part of the out-of-the-box NextGen deployment, however, NextGen is working on a project to take SETMA’s data-base and incorporate it into NextGen’s knowledge base. They will showcase their first version of that at the NextGen Annual User’s Meeting this October.
Question 1 Part III - IT Department
SETMA has six members of our IT Department. They operate and maintain a server-farm of overr 70 with over 60 software packages integrated. We have NextGen secure web portal and NextGen’s HIE. We also utilize the EMR at all local hospitals, 28 nursing homes, and five clinics.
Question Two -- How do you decide what tools to develop? For example, how did you decide it is worth the time/money/effort to develop a lipid disease management tool?
Question 2 - Part I - Deciding what to develop
The major problem with CDS is not deciding what to develop but deciding how to develop it. Content, display and function are key elements to that process. One of the principles which Peter Senge enunciated in The Fifth Discipline is, “The more complex a problem, the more systemic the solution must be.” He was not talking about computer systems but “systems thinking,” but the principle applies. The decision as to what to develop revolves around taking complex task and “making it easier to do it right rather than not to do it at all.” A second principle is to bring to bear upon a patient encounter not what I know or you know but bring to bear what is known.
On our website at www.jameslhollymd.com under Electronic Patient Management Tools, you can see tutorials on all of CDS materials. A good example is the Framingham Cardiovascular and Stroke Risk Assessment tool. In August, 2010, the American Family Physician (reference: Global Risk of Coronary Heart Disease: Assessment and Application, Anthony J. Viera, MD, MPH and Stacey L. Seridan, MD, MPH, University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, North Carolina Am Fam Physician. 2010 Aug 1;82(3):265-274) recommended that family physicians calculate one risk score for each of their patients every five years.
SETMA has always done several of these but deployed all twelve of them in 2010. Now, we do all twelve calculations every time we see a patient and the patient receives their results on their plan of care and treatment plan which is printed and given to the patient at the end of the visit.
In addition, we add a “What IF Scenario.” One of the calculators produced a “relative heart age.” It shows the patient’s “real heart age” which is their chronological age and then shows what their “relative heart age” is based on their condition. Our “What If” Scenario shows patients what their “relative heart age” is if they complete one of five improvements. In other words, we are able to show the patient that “If they make a change, it will make a difference.”
It would take a provider 30 minutes to calculate all of the scores by hand and it can take five minutes to do with it with a web-based tool, SETMA’s CDS, makes it possible to do all 12 scores in ONE SECOND, with the “What If Scenarios,” with adding the information to our plan of care and treatment plan to give to the patient.
Boiled Frog Analogy
The boiled-frog analogy has often been used to illustrate the reluctance of people to change their behavior because they are not uncomfortable. The analogy describes a frog which is placed in a pot of cool water. The frog is comfortable and senses no danger. When the pot is placed on a stove and heat is applied, the change is so gradual that the frog is not aware of the danger until it is too late. The frog boils to death.
This is not unlike a patient who complains, “But, I was fine yesterday, why am I unable to move my left arm today?” The reason is that the patient did not take their blood pressure medication and did not control their weight and did not stop smoking until it was too late. The cause of the stroke started many years before the actual event. By the way, it is NEVER -too late to begin making changes. Recent research has shown that smokers who are diagnosed with lung cancer live longer and are more comfortable if they stop smoking than are the patients who are diagnosed with lung cancer and continue to smoke. It is NEVER too late to quit smoking.
Creating Discomfort in Patients
The problem remains as to how to change patient behavior. This was a problem for providers as well. The tendency of healthcare providers not to -change,|| is called -treatment inertia. If is the inclination not to change things even when patients are not treated to goal. In addressing this, SETMA began publicly reporting provider performance by provider name. This created discomfort in the providers and has had a positive effect on the quality of care patients are receiving.
But, how do we make the patient uncomfortable enough that they will make and sustain changes in their lifestyles and compliance with a plan of care? One of the ways is with -risk stratification.
The calculation of a patient‘s risk of developing significant health problems and the showing of that calculation to the patient is one way SETMA attempts to encourage patients to make and sustain change. SETMA uses many tools to evaluate patient health risk. All are described on SETMA‘s website under the heading Electronic Patient Management Tools.
SETMA’s Innovative Use of the Framingham Risk
This tutorial explains the changes and use of SETMA‘s deployment of the 12 risk calculators published by the Framingham Heart Study. These tools are not absolute and must be used as an indication of potential cardiovascular and cerebrovascular risk and not as an absolute indicator of future disease.
One of the most interesting tools is the calculation of -relative heart age. It is explained below. This will be a useful tool for encouraging life-style modifications by patients but is only an indication and not an absolute assessment of -heart age.
The most innovative use of the Framingham Risk Calculators were suggested by SETMA‘s associates at the Diabetes Center of Excellence in Boston (SETMA is the only multi-specialty Affiliate of the Diabetes Center of Excellence).. Drs. Richard Jackson and Ken Snow, while visiting SETMA, recommended the adding of a -What If Scenario to our display of all twelve calculators.
If You Make a Change it Will Make a Difference
The concept is that we are asking patients to make changes which will not show up as benefits for decades. Of course, ignoring those changes will result in irrevocable deterioration in the patient‘s health over those decades. But how do you -prove to a patient that -if you make a change, it will make a difference? One way is with the Framingham Risk Calculators being presented to the patient with the inclusion of the changes which would result if the patient improved the elements of the risk calculator.
Even though these risk calculators are not perfect, they are still the best we have. And, it is imperative that patients know and that their provider knows what their risk is, because it is with the knowledge of the patient‘s cardiovascular risk that a plan of care and a treatment plan can be designed to help preserve the patient‘s health.
Remember, -Risk is an attempt to determine what the future might be like which means it is imprecise. Some people with a high risk will not experience poor health and some who have low risk will. Overall, however, those with high risk will have more heart attacks and strokes than those with low risk.
What If?
Because it takes SETMA only one second (really) to calculate all twelve risk calculators, we thought we were doing great. However, when we showed this function to our new colleagues from Joslin Diabetes Center, Dr. Richard Jackson commented that these scores overstate the risk and Dr. Kenneth Snow asked if we could show the patient how their risk would be affected if they make a change in their habits? Sadly, we had to admit that we could not. That was on Tuesday November 30, 2010.
We realized that while the patient has to know their risk, to understand -dynamic complexity and its dangers for their ignoring their health until it is too late, and to avoid -shifting the burden of responsibility from themselves to another, their healthcare providers have a responsibility to show them that if -they make a change that it will make a difference.
The General Cardiovascular Disease 10-Year risk
This score projects the probability of a person having a major cardiovascular event such as a heart attack or stroke in the next ten years. The above patient‘s -real heart age is 45 years but the -relative heart age is 80 years (his health is deteriorating more rapidly than he is aging), and the 10 year risk is high at 30%. These are very discouraging number for a 45 year old man. But now that we have added the -What If? section, we can assure this man that if he will make a change, it will make a difference. In addition, the greatest opportunity for improvement in his risk is indicated by the change in risk with each of the scenarios below.
- If he changes all of the elements in this calculation which are changeable (systolic blood pressure, cholesterol, smoking, hypertension treatment), his risk will improve. The unchangeable features are age, gender and diabetes.
- If he changes all of the elements to -evidenced-based goals, his risk will drop to 9.4% and his -relative heart age will drop from 80 to 54. These are dramatic improvements in his risk. We can categorically assure him that :if he makes a change, it will make a difference.”
- If he changes all of the elements by a 20% improvement, his risk will drop to 18.4% and his relative heart age will drop to 68. Obviously these are not as good as the result of treating him to goal, but they are significantly improved.
- The changes for treating his blood pressure to goal without affecting the other elements shows a drop in risk as does changing the cholesterol. There is no improvement for smoking cessation in that it is noted that this patient does not smoke.
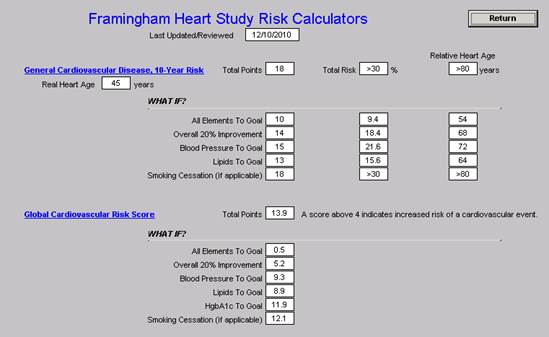
The other eleven scores are similarly described on the tutorial.
Plan of Care and Treatment Plan
If a patient is going to make a change which will make a difference, there must be a basis on which change can be expected. We know that conversations at the time of an office visit are part of that decision to make a change. However, without a written, personalized plan of care and treatment plan, few patients will successfully make those changes and sustain them.
The “WHAT-IF?” scenarios described above will be added to patients‘ diabetes, hypertension and/or lipid plans of care and treatment plans. These documents are the -batons which are passed from one member of the healthcare team - your healthcare provider - to another member of the team - the patient. If the patient will study these documents, we believe it will encourage them to make changes and it is our confidence that those changes will make a difference. With the patient‘s name and personal data in each plan, the probability of their studying the material is greatly increased.
Question 2 - Part II - Why is it worth the money to do CDS for lipids?
The complexity of a treatment protocol, guideline, algorithm or principle will give and the magnitude of the benefit a patient will receive from effective treatment of a condition will give a great deal of guidance to what CDS’ are worth developing. SETMA’s development of a Lipid Suite of Templates was actually a recruitment tool. One of our current partners was going to a residency program to teach. He had ties to our community and I promised him that if he would join us within two months we would build a lipid disease management tool. He joined us and we built it. A brief review of this took at Lipids Tutorial will let you see why it is so valuable. The computations needed for proper diagnosis and treatment of lipid disorders makes it an ideal subject for CDS.
Question Three -- Are the clinical decision support tools used on desktop computers in each exam room? Or Tablets that each nurse/physician carry throughout the day?
All CDS tools are available in all clinic rooms (over 100), 3 emergency departments, hospital wards (four hospitals), 28 nursing home, provider homes, hospice, home health, etc. so that no matter where a patient is seen, their encounter is completing in the same database of all other encounters. Because the core of CDS is the baton (see below), we have laser printers in every exam room to facilitate our giving patients their treatment plan and plan of care and the data analytics on their care. Our staff in the hospital and nursing homes often use laptops but we have CPU in every exam room. All of our providers also have access to the EMR via iPads, iPhones, Laptops, etc. wherever they are, including recently in Ireland. This is through Citrix.
The Baton
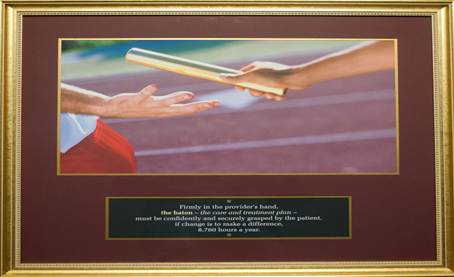
The attached is a picture of a framed copy of "The Baton." "The Baton" is a pictorial representation of the patient's "plan of care and the treatment plan," which is the instrument through which responsibility for a patient's health care is transferred to the patient. Framed copies hang in the waiting room of SETMA II and will soon hang in all public places throughout SETMA's clinics. A poster copy will be hung in every examination room. The poster declares:
Firmly in the providers hand
--The baton - the care and treatment plan
Must be confidently and securely grasped by the patient,
If change is to make a difference
8,760 hours a year. The poster illustrates:
- That the healthcare-team relationship, which exists between the patient and the healthcare provider, is key to the success of the outcome of quality healthcare.
- That the plan of care and treatment plan, the "baton," is the engine through which the knowledge and power of the healthcare team is transmitted and sustained.
- That the means of transfer of the "baton" which has been developed by the healthcare team is a coordinated effort between the provider and the patient.
- That typically the healthcare provider knows and understands the patient's healthcare plan of care and the treatment plan, but that without its transfer to the patient, the provider's knowledge is useless to the patient.
- That the imperative for the plan - the "baton" - is that it be transferred from the provider to the patient, if change in the life of the patient is going to make a difference in the patient's health.
- That this transfer requires that the patient "grasps" the "baton," i.e., that the patient accepts, receives , understands and comprehends the plan, and that the patient is equipped and empowered to carry out the plan successfully.
- That the patient knows that of the 8,760 hours in the year, he/she will be responsible for "carrying the baton," longer and better than any other member of the healthcare team.
The genius and the promise of the Patient-Centered Medical Home is symbolized by the "baton." Its display will continually remind the provider and will inform the patient, that to be successful, the patient's care must be coordinated, which must result in coordinated care. In 2011, as we expand the scope of SETMA's Department of Care Coordination, we know that coordination begins at the points of "transitions of care," and that the work of the healthcare team - patient and provider - is that together they evaluate, define and execute that care.
Question 3 -- How much has SETMA invested in CDS tools?
SETMA is debt free. We are also totally dependent upon our own productivity. We have no grant or foundation support. In fact, SETMA has its own foundation through which we pay for the care of our patients who di help None of the Foundation’s money can be paid to SETMA. Annually, the SETMA partners give $500,000 to the SETMA Foundation. We have seen miracles in people’s lives as we are able to get them the care they need and could not otherwise support. As we use CDS and technology, we never forget that we are dealing with real people with real problems.
SETMA has invested over $8,000,000 in IT and at least $3,000,000 of that has been in the building and deployment of clinical decision support.
Question Four -- How have SETMA's CDS tools affected the overall cost of care? (For example, improved blood sugar levels for diabetic patients obviously reduces the cost of their care over their lifetimes. Have you considered the big-picture savings that could be attributed to your CDS tools?)
This is a difficult question. It is hard to separate the value of CDS from the value of the underlying EMR. We last did an ROI evaluation on our practice in regard to electronics over ten years ago. At that time it was a very positive figure. The efficiency of having the same data base and the same management tools at every venue we see our patients is immeasurably valuable. When you analyze Value as a function of Quality divided by Cost, you can increase Value by either increasing Quality or decreasing cost or both.
We know that our mean HbA1C - the means by which we measure the quality of our care of patients with diabetes - improved by .3 percent from 2000 to 2001 and from 7.54% to 6.64% between 2000 and 2011. We know that this saved the sight, kidneys and hearts of many patients but we don’t have verifiable data on that. Our Standard Deviation for HbA1C changed from 1.98 in 2000 to 1.20 in 2011. This means that our population health has improved dramatically as well as individual health. SETMA is the only multi-specialty practice which is an Affiliate of the Diabetes Center of Excellence at Harvard University. We are also an NCQA PC-MH.
We use Business Intelligence to look for leverage points to improve care by looking at the differences between patients who are treated to goal and those who are not. It must be remember, initially as the quality of care goes up, the cost will go up. The first year, SETMA got serious about immunizations, we spent $1,000,000 on buying immunizations. Because many of those are every ten years that initial investment has paidoff in the next nine years as the costs dropped dramatically.
Question Five -- How does the use of the pre-visit preventive and screening tool and the LESS Initiative tool affect work flow? Did you add staff to administer these tools before the patient visits the physician? How long does it take to administer each tool?
Question 5 - Part I - Work Flow
The Pre-visit and LESS speed things up rapidly. In less than five seconds a nurse can visually see what prevention or screening needs the patient has. With the one click ordering capacity, completing those is very fast. The LESS takes about 27seconds to caccomplish and provides each patient with a written personal weight management assessment, a personal exercise prescription and a persona evaluation of smoking cessation needs.
I recently spoke to the Massachusetts Medical Society. Another speaker asked the questions, “How many tasks can you get a doctor to perform?” He said, he thought about one. When I spoke, I started by answering his questions, I said, “It depends upon how long it takes. If you take a complex task and make it easy to do, i.e., in less than one second, you can get a provider to do 15 or twenty tasks, particularly when the completion of those tasks adds great value to the patient’s care.” Of course, when you are working in teams, the synergism increases the collective capacity of the group.
Question 5 - Part II - Adding staff
We did not add staff to do the CDS support although we have added staff for care coordination care transitions.
Question 5 - Part III - How long does it take to administer each tool
- LESS - 27 seconds
- Preventive and Screening - five seconds
- Framingham - 1 second
- Cardiometabolic Syndrome screening - one second
- HEDIS Measures review - five seconds
- Many more
Question Six -- How does the use of the disease management tools affect work flow? Do they affect the average length of an office visit?
Question 6 - Part I - Affect Work Flow
Because the tools perform complex tasks simply such as producing a Plan of Care and Treatment Plan which is unique to the individual patient, with their name on each patient and their data analysis throughout the document, they improve workflow and make it easier and faster to “pass the baton” to the patient.
Question 6 - Part II - Affect average length of an entire visit
Looked at as a discrete process, it will affect it by 2-3 minutes if three disease management tools are used with each patient. When look as an overall function is saves twenty minuets or more per visit.
Question Seven -- How have SETMA physicians reacted to the emergence of CDS tools? Universal enthusiasm? Reluctance to comply? Reticence about public reporting? Have you had any turnover among your physician or nursing colleagues that is attributable to your use of CDS tools?
Question 7 Part I - Providers reacting
Because we close our clinic one a month and spend 3-4 hours in training, there is excellent acceptance, although there are still discernible differences in the performance of some providers, the key for providers is like that for patients, if you ask them to make a change in work flow, it had better make a difference. Because of our deployment method for CDS, always making it easier to do it right than not do it at all and bringing to bear what is known, all of our providers and nurses, and support staff and administration, very much value our CDS.
Question 7 Part II - Universal Enthusiasm
With the national recognition SETMA has received for our CDS (see Award on our website) our providers have been enthusiastic. They like the recognition which is a powerful tool for change in a provider’s performance. Also, because we publicly report on over 250 quality metrics by provider name and because our CDS aids the provider in performing well incidental to excellent care, they are enthusiastic. Clinical inertia goes away with public reporting. Said another way, “Once you ‘open your books on performance’ to public scrutiny, the only safe place you have in which to hide is excellence.”
Question 7 Part III Reluctance to Comply
There is not reluctance because we have a celebratory and collaborative managerial model, with leadership setting the example. Others do what they should because those who are encouraging them are aleady doing it.
Question 7 Part IV - Any Turnover
In 1999, we had one part-time physician who left because of the newly deployed EMR. Two weeks later he wanted to come back and we said no. In 2004, we had a physician who was careless with his work and we dismissed him.
Question Eight - What have been the biggest challenges to using CDS tools? How have you addressed those challenges?
Question 8 - Part I - biggest challenge
Getting the content right. For instance, we took the National Kidney Foundation’s 460-page summary of renal disease and educed it to CDS. We took the AMA’s 220 page Adult Weight Management notebook and reduce it to a CDS. We chose to build the entire suite and then to have two plans of use: one is the full version which might take 30 minutes and be exhaustive if not exhausting; the short version which allows excellent analysis but takes on a minute. The mistake would be to assume that unless the entire CDS is used very time, it does not have value.
Question 8 - Part II - addressing challenges
Sharing a vision for improvement of care via CDS, then finding ways to employ a CDS tool in a manageable work flow with value to the patient is the key. In our monthly training sessions we discuss work flow modifications which allows a provider to work within the time constraints we all have and still practice excellent medicine with CDS.
Question Nine -- What have been the biggest rewards/benefits of using CDS tools?
The rewards have been improvement in the care we deliver and the ability to prove that we have improved that care. CDS support have allows us to become Tier III NCQA Patient-Centered Medical Home and AAAHC Ambulatory Care Certified and a Medical Home. It has allowed us to meet NCQA Diabetes recognition standards, to win the HIMSS Davies award, to be name by ONC as one of 30 Exemplary practices in CDS, to have AHRQ publish our LESS Initiative on their Innovations Exchange and many others.
But the biggest reward is our ability to know what we are doing and know that we are doing it well and that it is excellent.
Question Ten -- What "lessons learned" can you share with other healthcare leaders that want to increase the use of CDS in the outpatient setting?
In his seminal work, The Fifth Discipline, Dr. Peter Senge addresses “systems thinking.” While the term does not refer to computer systems, the principles apply to health care delivery via an electronic format as legitimately as to other business enterprises.
Senge states, “Learning has come to be synonymous with ‘taking in information.’...Yet, taking in information is only distantly related to real learning.” Classically, healthcare has focused upon “taking in information” in the form of facts. The hurdle required to enter medicine as a physician is the proven ability to absorb and retain tens of thousands of isolated pieces of information and then to be able to repeat that information in a test format. Clinical training attempts to take the static database created by these facts and transform it into a dynamic tool which can provide answers to complex disease-process questions. This is where the complexity comes into healthcare: how do you take a linear database and transform it into a circular, global, decision-making tool?
Senge also identified the problem with which healthcare is faced today. He stated: “System thinking is needed more than ever because for the first time in history, humankind has the capacity:
- To create far more information than anyone can absorb,
- To foster far greater interdependency than anyone can manage
- To accelerate change far faster than anyone’s ability to keep pace.”
Undermining Confidence
Senge concludes, “Complexity can easily undermine confidence and responsibility.” Confidence is undermined when the vastness of available, valuable and applicable information is such that it appears futile to the individual to try and “keep up.” In healthcare, once confidence is undermined, responsibility is surrendered as providers tacitly ignore best practices, substituting experience as a decision-making guide. While experience is not without merit in medical decision making, it is not the best guide.
Any sense of healthcare provider helplessness has a solution, but it is not based on attempting to take in more and more information. Senge states, “Systems thinking is the antidote to this sense of helplessness that many feel as we enter the ‘age of interdependence.’” The solution is not only to “see” the interrelatedness of disease-processes, one disease aggravating or precipitating another, but also to see the dynamic interaction between the treatments of two or more simultaneously occurring pathological processes. The solution also allows the healthcare provider to “see” how the treatment of one disease processes is required in order to augment and/or to facilitate the treatment of another.
CDS can relieve a great deal of frustration. It can allow a group of providers to update their knowledge and skills routinely. For instance, annually, the American Diabetes Association published a 100-page update on quality of care in diabetes. It really is not possible for every provider in an organization to read this, but if one will and then if that one will update the CDS and Disease management tool, then all can practice with that knowledge.
|